How We End Up Developing Type 2 Diabetes
Get Personalized Insights
How We End Up Developing Type 2 Diabetes
Type 2 diabetes is a condition that can be reversed in a significant proportion of patients through appropriate medical supervision and targeted changes in lifestyle and diet.
Diabetes represents a group of metabolic disorders primarily caused by insulin dysfunction. Insulin is the hormone that acts as a key, allowing glucose (sugar) to enter cells.
Globally, nearly one in nine adults (589 million) are now living with diabetes, while in the United States more than one in three adults is in a pre-diabetic stage. In the UK, more than 5.8 million people in the UK are living with diabetes, while an estimated 1.3 million remain unaware of their condition.
Type 1 diabetes, or juvenile diabetes, is characterized by low or nearly absent insulin secretion. In contrast, type 2 diabetes is characterised, for an extended period, by excessive insulin secretion.
In its early stages, insulin levels are elevated as the body attempts to maintain normal blood glucose. Prolonged overproduction of insulin leads to cellular resistance to its action. Gradually, cells become less responsive to insulin’s signal to absorb glucose (Figure 1).
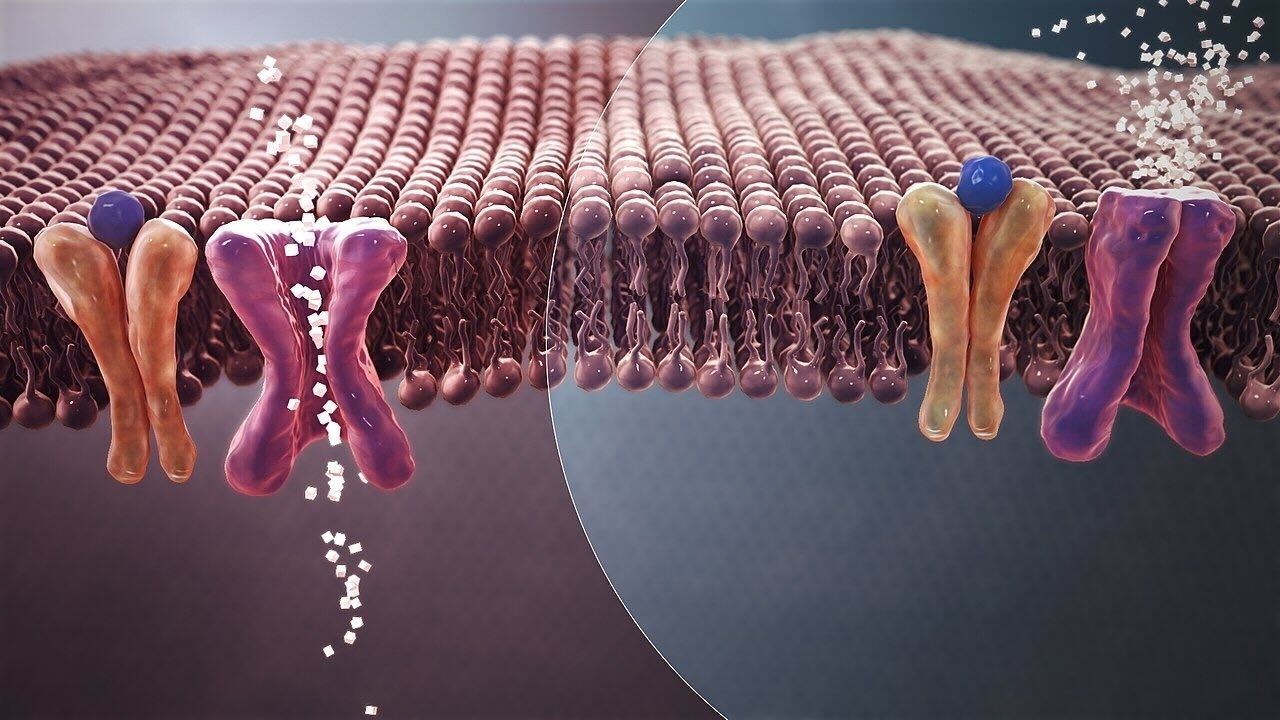
As cells fail to respond effectively to insulin, the pancreas compensates by producing increasing amounts of it. Over time, this constant demand exhausts the pancreas, leading to reduced insulin production. At that point, blood sugar levels begin to rise, and diabetes is diagnosed.
The initial stage of excessive insulin secretion is called pre-diabetes or metabolic syndrome. This phase typically lasts several years before pancreatic exhaustion and elevated blood glucose become apparent.
Type 2 diabetes is almost entirely the result of modern lifestyle and dietary habits. Until the early 1960s, it was a relatively rare disease [3–5].
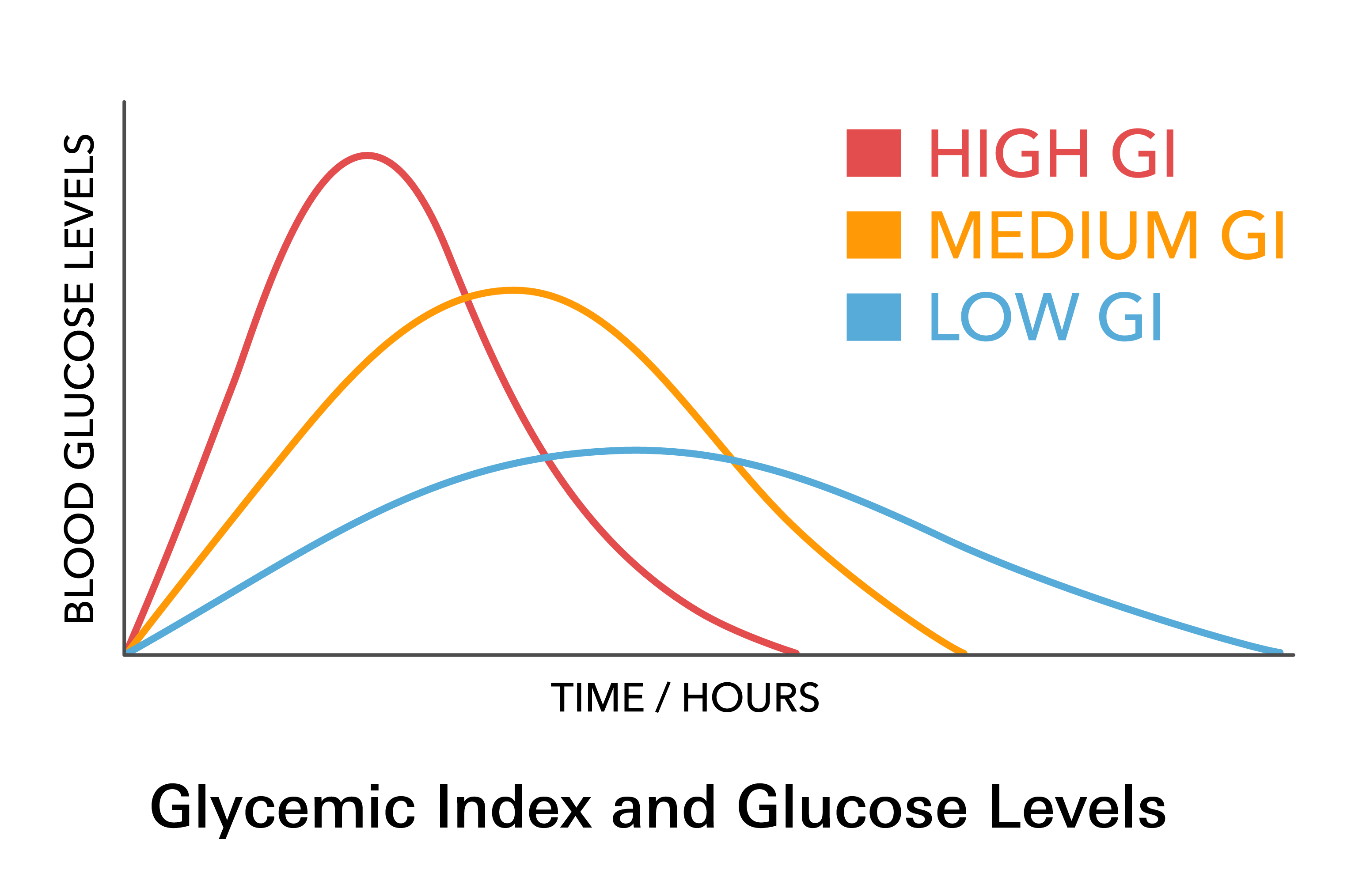
Modern dietary patterns and sedentary behaviour play a central role in the development of diabetes. Highly processed foods cause sharp spikes in blood glucose, triggering the secretion of large amounts of insulin (Figure 2). By contrast, unprocessed foods are absorbed more slowly, do not cause abrupt glucose surges, and therefore require less insulin for metabolism [4–7].
For millions of years, until only a few decades ago, humans lived in environments where food was scarce and significant physical effort was required to obtain it. Our hormonal system is therefore genetically programmed to function optimally with foods rich in nutrients but relatively low in calories.
Modern humans, however, move less while consuming increasing amounts of highly processed foods, thereby worsening insulin resistance. In contrast, physical activity enhances cellular glucose uptake, lowers blood sugar, and reduces insulin resistance.
The modern lifestyle promotes diabetes through multiple mechanisms [1–3]:
- Highly processed foods [4–7].
- Low physical activity [8].
- Vitamin and micronutrient deficiencies [9–13].
- Living in enclosed spaces linked to low vitamin D levels.
- Alteration of the microbial flora (antibiotic overuse, food preservatives, overconsumption of sugar and alcohol) [14].
- Stress (increased levels of stress hormones such as cortisol and adrenaline promote insulin resistance) [15,16].
The most common approach is to take medication to lower blood sugar levels and delay the onset of complications from the disease.
Although pharmacological approaches achieve some risk reduction, it cannot restore the wide range of metabolic disorders present in diabetes.
Unfortunately, insufficient emphasis has been placed on addressing the reversible factors that cause diabetes. This approach is reinforced by the belief that type 2 diabetes is irreversible and requires continuous drug therapy to counter the gradual decline in pancreatic function [1].
However, evidence from numerous studies in patients with type 2 diabetes shows that intensive lifestyle and dietary interventions, combined with weight loss, improve blood glucose control, reduce medication requirements, and can lead to diabetes remission [1,17–22].
Another reason is that the metabolic disturbances of diabetes and pre-diabetes often go unnoticed, as they do not immediately manifest as disease-specific symptoms.
Symptoms caused by diabetes include:
- Irritability and aggression
- Severe fatigue
- Weakness
- Drowsiness and decreased clarity
- Erectile dysfunction or impotence
- Intense hunger
- Constipation and digestive disorders
- Frequent urination
- Blurred vision
- Delayed wound healing
- Numbness and tingling in the hands and feet
- Fungal infections
- Skin problems (pallor, itching, darkening of areas such as the armpits and groin)
- Nightmares or crying during sleep
- Headaches
- Tachycardia
- Increased sweating
These symptoms are often perceived as “normal” effects of age, overwork, stress, or indigestion after a heavy meal. As a result, they are rarely recognised by patients as manifestations of diabetes.
Type 2 diabetes causes serious complications, diminishes quality of life, and markedly increases the risk of morbidity and mortality from [23,24]:
- Cardiovascular diseases
- Cancer
- Kidney failure
- Diabetic retinopathy
- Pneumonia
- COVID-19
In recent years, type 2 diabetes has increasingly affected younger adults aged 18–50 years, who experience more severe complications and reduced life expectancy [1].
Halting the Progressive Deterioration of Type 2 Diabetes
Type 2 diabetes is reversible in a substantial proportion of patients under appropriate medical supervision and through targeted lifestyle and dietary changes.
Clinical experience shows that identifying and correcting deficiencies that negatively affect the metabolic profile of individuals with diabetes helps restore health more effectively [5,25–27].
Correcting insulin resistance is essential for:
- Type 2 diabetes treatment
- Body weight reduction
- Improved quality of life
- Reduced risk of diabetes complications (affecting the heart, blood vessels, kidneys, etc.)
- Reduced chronic inflammation
- Improved overall health in patients with diabetes and metabolic syndrome
Medication, correction of deficiencies, and diet must be tailored to each patient’s metabolic profile. This personalisation allows changes and improvements to be sustained long term.
A simple reduction in calorie intake that does not account for individual metabolic differences is particularly difficult to maintain due to hunger and fatigue. The use of specialised dietary approaches that prevent increased hunger and fatigue supports long-term adherence to lifestyle changes [17,20].
Specialised Tests for Diabetes & Insulin Resistance Care
Identifying and correcting metabolic dysfunction requires comprehensive lab testing that detect metabolic disorders associated with diabetes and insulin resistance that influence the onset and progression of autoimmune and chronic diseases.
An individual’s metabolic status is the primary risk factor for the manifestation of these conditions.
This type of analysis is not comparable to routine checkups. These are highly specialised and comprehensive tests. Kyma offers this level of comprehensive, advanced lab testing by partnering with leading, certified partner labs.
Key Factors Identified by Kyma’s Comprehensive Lab Testing
Kyma's comprehensive lab panel identifies key indicators, including:
- Deficiencies in vitamins, enzymes, minerals, amino acids, and omega-3 fatty acids
- Metabolic disorders such as insulin resistance
- Capacity to regulate inflammation
- Antioxidant capacity
- State of the intestinal microbiome
- Fatty acid metabolism and metabolising simple sugars
- Hormonal imbalances
Conventional methods make it difficult to precisely detect individual deficiencies. As a result, correction typically relies on general recommendations. With in-depth lab testing, we can now accurately identify the body's deficiencies and metabolic dysfunctions that deteriorate quality of life.
This serves as an additional diagnostic tool that guides the targeted correction of deficiencies using therapeutic doses of micronutrients.
Medication, coordinated with the individual’s primary care provider, along with correction of deficiencies and diet, should be tailored to each person’s metabolic profile. This personalisation sustains improvements over time.
Because the development of type 2 diabetes and pre-diabetes is driven by lifestyle, diet, and nutritional deficiencies, precise interventions in these areas—through lifestyle optimization, correction of deficiencies, and proper nutrition—can reverse the course of the disease and radically change the health trajectory of individuals with type 2 diabetes, pre-diabetes, and insulin resistance [1,27–31].
References:
- Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): an open-label, parallel-group, randomised controlled trial. Shahrad Taheri, Hadeel Zaghloul et. al. www.thelancet.com/diabetes-endocrinology Vol 8 June 2020.
- Type 2 Diabetes Mellitus Epidemiology. https://emedicine.medscape.com/article/117853-overview#a5.
- Long-term Trends in Diabetes April 2017 CDC report. https://www.cdc.gov/diabetes/statistics/slides/long_term_trends.pdf
- Hidden Hunger: Strategies to Improve Nutrition Quality. H.K. Biesalski, R. Birner. Basel, Karger, 2018, vol 118, pp 131–143. https://www.karger.com/Book/Toc/276874
- Anthropogenic Pressure and Lifestyle are the Underlying Cause of Pandemic Chronic Diseases. Dimitris Tsoukalas, Evangelia Sarandi, Aristides Tsatsakis, Daniela Calina. Journal of Siberian Federal University. Biology 2019-09.
- Understanding Empty Calories. Harvard Medical School
- Environmental/lifestyle factors in the pathogenesis and prevention of type 2 diabetes Hubert Kolb and Stephan Martin. BMC Med. 2017; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5516328/
- Exercise and Type 2 Diabetes The American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010 Dec. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2992225/
- Sugar isn’t just empty, fattening calories – it’s making us sick. Robert Lustig. October 27, 2015. https://theconversation.com/sugar-isnt-just-empty-fattening-calories-its-making-us-sick-49788
- Potential micronutrient deficiency lacks recognition in diabetes Ann F Walker. Br J Gen Pract. 2007. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2032692/
- Micronutrient Status in Type 2 Diabetes: A Review Bhupinder Kaur, Jeyakumar Henry. Adv Food Nutr Res . 2014. https://pubmed.ncbi.nlm.nih.gov/24484939/
- Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. Bruce N. Ames. PNAS 2006. https://www.pnas.org/content/pnas/103/47/17589.full.pdf
- Prolonging healthy aging: Longevity vitamins and proteins Bruce N. Ames PNAS October 23, 2018. https://www.pnas.org/content/115/43/10836.
- Type 2 diabetes and gut microbiome: at the intersection of known and unknown Smitha Upadhyaya* and Gautam Banerjee. Gut Microbes. 2015. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4615359/
- Stress increases the risk of type 2 diabetes onset in women: A 12-year longitudinal study using causal modelling Melissa L. Harris. PLoS One. 2017 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5319684/
- Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus Joshua J. Joseph and Sherita H. Golden. Ann N Y Acad Sci. 2017 Mar. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5334212/
- Taylor R, Al-Mrabeh A, Sattar N. Understanding the mechanisms of reversal of type 2 diabetes. Lancet Diabetes Endocrinol 2019; 7: 726–36.
- Type 2 diabetes is a reversible condition. Roy Taylor, Newcastle University. Science Daily. September 13, 2017. https://www.sciencedaily.com/releases/2017/09/170913084432.htm
- Reversing Type 2 Diabetes: A Narrative Review of the Evidence. Sarah J Hallberg et.al. Nutrients. 2019 Apr https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6520897/
- Calorie restriction for long-term remission of type 2 diabetes Roy Taylor. Clin Med (Lond). 2019 Jan. .https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6399621/
- ‘Reversing type 2 diabetes starts with ignoring the guidelines’. Sarah Hallberg. BMJ British Journal of Sports Medicine. July 2018. https://bjsm.bmj.com/content/bjsports/52/13/869.full.pdf
- Translating aetiological insight into sustainable management of type 2 diabetes Roy Taylor & Alison C. Barnes Diabetologia, November 2017. https://link.springer.com/article/10.1007/s00125-017-4504-z
- Type 2 Diabetes Mellitus. Prognosis. https://emedicine.medscape.com/article/117853-overview#a6
- 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD European Heart Journal, Volume 41, Issue 2, 7 January https://academic.oup.com/eurheartj/article/41/2/255/5556890#202785299
- Do flavanols-rich natural products relieve obesity-related insulin resistance? Ayse Basak Engin, Aristidis M Tsatsakis, Dimitris Tsoukalas, Atilla Engin. Food Chem Toxicol . 2018.https://pubmed.ncbi.nlm.nih.gov/29288757/
- Clinical aspects of precision medicine using as biomarkers telomere length, fatty acids and organic acids D Tsoukalas TOXICOLOGY LETTERS 314, S29-S29 https://www.sciencedirect.com/science/article/abs/pii/S0378427419302486?via%3Dihub
- World aging population, chronic diseases and impact of modifiable-metabolic risk factors. Dr. Dimitris Tsoukalas, MD (Greece). European Institute of Nutritional Medicine, E.I.Nu.M. 20th International Congress of Rural Medicine 2018. Tokyo - Japan.
- Chronic Inflammation in the Context of Everyday Life: Dietary Changes as Mitigating Factors. Margină, D.; Ungurianu, A.; Purdel, C.; Tsoukalas, D.;
Sarandi, E.; Thanasoula, M.; Tekos, F.; Mesnage, R.; Kouretas, D.; Tsatsakis, A. Int. J. Environ. Res. Public Health 2020, 17, 4135. - Metabolomics Signatures in Type 2 Diabetes: A Systematic Review and Integrative Analysis Yue Sun et al. The Journal of Clinical Endocrinology & Metabolism, April 2020
- Metabolic profiling of organic and fatty acids in chronic and autoimmune diseases. Evangelia Sarandi, Dimitris Tsoukalas et al. Advances in Clinical Chemistry. July 15, 2020. Elsevier Inc.
- Targeted Metabolomic Analysis of Serum Fatty Acids for the Prediction of Autoimmune Diseases. Tsoukalas, D, Saranti E, Fraggkoulakis V, et al. Front. Mol. Biosci. 6, 1–14 (2019).
- Image credits: Jiaqi Wang, The New York Times





