Multiple Sclerosis: How Metabolic Disorders and Deficiencies Are Linked to the Disease
Get Personalized Insights

Multiple Sclerosis: How Metabolic Disorders and Deficiencies Are Linked to the Disease
Multiple sclerosis (MS) is a chronic inflammatory neurological disease that affects the brain and spinal cord.
It is an autoimmune condition in which the immune system fails to recognise the protective sheath of nerves—myelin—as self tissue and consequently attacks and destroys it.
Patients with MS present metabolic disorders that aggravate the degeneration of nervous tissue.
Deficiencies in the body and metabolic disorders are a significant factor in both the development and progression of MS. Only in recent years has the extent to which metabolism influences immune system regulation—and contributes to autoimmune diseases such as MS—been fully recognised.
Over the last five years, metabolic processes have been highlighted as a central factor in the development of MS and autoimmune diseases in general.
This shift represents an important advancement in the fight against multiple sclerosis, offering deeper insight into the mechanisms driving the disease and contributing to improved therapeutic approaches.
The metabolic disorders associated with the onset and worsening of MS include:
- Deficiencies in micronutrients, vitamins, minerals, amino acids, omega-3 fats, and antioxidants
- Insulin resistance and impaired glucose metabolism
- Deregulated inflammatory responses
- Alterations in the microbial flora
- Dysfunction of myelin repair mechanisms
- Impaired energy production (mitochondrial dysfunction)
- Disruptions in lipid metabolism
- Increased oxidative stress
These metabolic disorders are directly linked to disease progression and the shift from the relapsing–remitting form of MS to the progressive form.
Patients with MS experience metabolic disorders that further exacerbate the degeneration of nervous tissue.
Early detection and targeted intervention of metabolic disorders play a crucial role in disease management and can help delay symptom progression and improve the quality of life of individuals living with MS.
An individual’s metabolic status is shaped by multiple factors, including:
- Lifestyle
- Diet
- The state of the microbial flora
- Medication
- The toxic load of the body (heavy metals, industrial chemicals)
- Exposure to microbial pathogens
- Stress
Vitamin D, the state of the bacterial flora, and omega-3 fatty acids are metabolic risk factors with particular importance in the pathogenesis of MS.
They are directly related to the development of myelin damage, the management of inflammation, and the regulation of the immune system.
It is encouraging that these are modifiable risk factors. Their improvement is directly linked to the course of the disease.
Vitamin D
Vitamin D is a key factor in all autoimmune diseases and especially in MS. High doses of vitamin D have an immunoregulatory effect. They reduce the factors that cause inflammation (interleukin-17) and enhance the mechanisms that control the body’s immune response (CD4+ memory).
Researchers from Johns Hopkins, Duke University, and Stanford published in Neurology the results of a study on the administration of vitamin D to two groups of patients with multiple sclerosis.
One group received low-dose vitamin D, while the other received higher doses, 10,400 IU for 6 months.
The average blood vitamin D level of those who received 800 IU remained very low (6.9 ng/ml), whereas the average level of those who received the higher dose was significantly elevated (34.9 ng/ml).
The study found that high doses of vitamin D are safe and have a strong immunoregulatory effect in patients with multiple sclerosis.
Adequate levels are essential for the proper functioning of the immune system—both for reducing susceptibility to infections and for enabling the immune system to correctly recognise the body’s own tissues. Low vitamin D levels are associated with more frequent relapses and a more severe course of MS.
Patients suffering from autoimmune disease often show resistance to vitamin D and therefore require larger doses and higher serum levels to achieve the same biological effect.
Vitamin D enhances the immune system’s ability to fight pathogenic viruses and microbes while restoring the body’s ability to recognise its own cells and tissues.
Reaching optimal vitamin D levels should be a priority in both prevention and management of MS. Measurement of 25-OH-D3 levels should be performed in all patients with autoimmune disease.
It is noteworthy that patients suffering from autoimmune disease often show resistance to vitamin D and therefore require larger doses and higher serum levels to achieve the same biological effect.
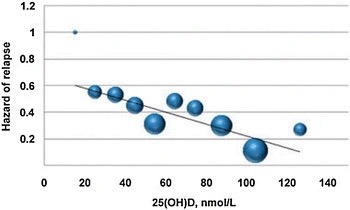
Studies have shown that as vitamin D levels increase:
- The likelihood of relapse decreases. An increase of 20 ng/ml reduces relapse risk by 50%.
- The risk of new lesions decreases. For every 10 ng/ml increase in blood vitamin D levels, the likelihood of detecting a new lesion on MRI drops by 15%, while the likelihood of detecting an active lesion drops by 32%.
To gain the full benefit of vitamin D, the body must also maintain adequate levels of the micronutrients that support its function. These micronutrients, known as vitamin D cofactors, include:
- Vitamin K2
- Zinc
- Boron
- Magnesium
- Calcium
- B-complex vitamins
Patients with MS often require higher doses than healthy individuals to achieve the maximum biological effect.
This needs to be carried out under medical supervision with a PCP and guided by blood tests that monitor the body’s response.
In recent years, a significant number of studies have shown that maintaining adequate vitamin D levels can have a protective effect and reduce the risk of developing multiple sclerosis.
Individuals with greater sun exposure and higher vitamin D levels have a lower risk of developing MS. Vitamin D supplementation is considered an important factor in lowering the risk of MS.
Specialised Tests That Detect Deficiencies & Metabolic Disorders Redefine the Care of MS
It is vital, in parallel with or following the diagnosis of the disease, to identify and manage the underlying metabolic disorders and risk factors that lead to its occurrence.
The earlier the metabolic disorders associated with MS are managed, the more effective the prevention and treatment interventions are.
The detection and treatment of metabolic disorders associated with MS are achieved by performing special tests that measure profiles metabolic status, inflammation levels, and micronutrient levels.
These are tests detect metabolic disorders and precise deficiencies associated with the onset of multiple sclerosis.
Addressing these metabolic disorders—through targeted lifestyle interventions, correction of deficiencies, and appropriate medications prescribed by one’s physician to control inflammation—can lead to better clinical outcomes and an improved quality of life for patients.
Restoring the body’s metabolic balance, combined with the implementation of targeted intervention in lifestyle and nutrition, improves the clinical picture and the health trajectory of patients with MS.
New evidence confirms that to achieve substantial improvement in health and quality of life for patients with autoimmune disease, each patient must be treated as a unique case.
The metabolic disorders and deficiencies in essential nutrients that led to disease onset must be corrected.
Medication, correction of deficiencies, and nutrition must all be tailored to each patient’s unique metabolic profile. This personalized approach helps ensure that improvements are sustained over the long term.
By measuring multiple biomarkers across more than 12 core body systems, we can identify the specific interventions each patient needs to positively influence the course of the disease.
Although there is no permanent cure for MS, our clinical experience shows that controlling symptoms while simultaneously correcting the underlying metabolic disorders can substantially improve patients’ overall health, enhance symptom control, and reduce the frequency of relapses.
Bibliographic References
[1] Multiple sclerosis. Mayo Clinic. Accessed Jan 2021.
[2] Multiple Sclerosis. Author: Christopher Luzzio. Emedicine Medscape. Updated Sep 02 2020.
[3] Multiple Sclerosis: Why Are Women More at Risk? Johns Hopkins Medicine. Accessed Jan 2021.
[4] Multiple Sclerosis Prof Alan J Thompson et al. THE LANCET. March 2018
[5] The Mechanism of Action of Interferon-β in Relapsing Multiple Sclerosis. Bernd C. Kieseier. CNS Drugs, Springer. August 2012.
[6] Mitoxantrone (Rx). Medscape.
[7] For RMS patients on Aubagio, elimination can be accelerated. Sanofi Genzyme, 2019.
[8] Drug Approval Package: ZEPOSIA. U.S. Food & Drug Administration. March 2020.
[9] Impact of Exercise on Immunometabolism in Multiple Sclerosis. Remsha Afzal et al. J Clin Med. 2020 Sep.
[10] A guide to immunometabolism for immunologists. O’Neill LA, Kishton RJ, Rathmell J. Nat Rev Immunol. 2016.
[11] Serum Compounds of Energy Metabolism Impairment… in Multiple Sclerosis. Giacomo Lazzarino et al. Mol Neurobiol. 2017 Nov.
[12] A blood-based metabolomics test to distinguish relapsing-remitting and secondary progressive multiple sclerosis: addressing practical considerations for clinical application.Tianrong Yeo et al. Nature Scientific Reports. 24 July 2020.
[13] Metabolomic signatures associated with disease severity in multiple sclerosis. Pablo Villoslada et al. Neurol Neuroimmunol Neuroinflamm. 2017.
[14] Disability in patients with multiple sclerosis: Influence of insulin resistance, adiposity, and oxidative stress. Sayonara Rangel Oliveira et al. Nutrition. March 2014.
[15] Metabolic pressure and the breach of immunological self-tolerance. Veronica De Rosa et al. Nature Immunology. October 2017.
[16] Prediction of Autoimmune Diseases by Targeted Metabolomic Assay of Urinary Organic Acids. Dimitris Tsoukalas et al. Metabolites. Dec 2020.
[17] Metabolomic profile of insulin resistance in patients with multiple sclerosis is associated to the severity of the disease. Alejandro Ruiz-Argüelles et al. Mult Scler Relat Disord. 2018.
[18] Metabolic defects in multiple sclerosis. Reginald C. Adiele, Chiedukam A. Adiele. Mitochondrion. 2019.
[19] Metabolic alterations in multiple sclerosis and the impact of vitamin D supplementation. Bhargava P et al. JCI Insight. 2017.
[20] Metabolomics in multiple sclerosis disease course and progression. Pavan Bhargava, Daniel C. Anthony. Multiple Sclerosis Journal. Jan 22, 2020.
[21] Metabolism as a Target for Modulation in Autoimmune Diseases. Nick Huang, Andras Perl. Trends in Immunology. May 05, 2018.
[22] Safety and immunologic effects of high- vs low-dose cholecalciferol in multiple sclerosis. Sotirchos ES, Bhargava P et al. Neurology. 2016 Jan.
[23] Micronutrient deficiencies in patients with COVID-19: how metabolomics can contribute to their prevention and replenishment. Dimitris Tsoukalas & Evangelia Sarandi. BMJ Nutrition Prevention & Health. Nov 2020.
[24] Vitamin D and Multiple Sclerosis: A Comprehensive Review. Martina B. Sintzel, Mark Rametta, Anthony T. Reder. Neurol Ther. 2018 Jun.
[25] Vitamin D and MS: Is there any connection?. Mayo Clinic. Accessed Jan 2021.
[26] Gut bacteria from multiple sclerosis patients modulate human T cells and exacerbate symptoms in mouse models. Egle Cekanaviciute et al. PNAS. 2017.
[27] Impact of microbiota on central nervous system and neurological diseases: the gut-brain axis. Qianquan Ma et al. Journal of Neuroinflammation. March 2019.
[28] The Central Nervous System and the Gut Microbiome. Gil Sharon et al. Cell. Nov 2016.
[29] Immunomodulatory and anti-inflammatory effects of probiotics in multiple sclerosis. Mohammad Morshedi et al. Journal of Neuroinflammation. Nov 2019.
[30] Gut microbiome of treatment-naïve MS patients of different ethnicities early in disease course. R. E. Ventura et al. Nature Scientific Reports. Nov 2019.
[31] Microbiome in Multiple Sclerosis: Where Are We, What We Know and Do Not Know. Marina Kleopatra Boziki et al. Brain Sci. 2020 Apr.
[32] Nutritional factors and aging in demyelinating diseases. Ana M. Adamo. Genes & Nutrition. Springer, 2014.
[33] Analysis of the intricate effects of polyunsaturated fatty acids and polyphenols on inflammatory pathways. Denisa Margină, Dimitris Tsoukalas, Aristides Tsatsakis et al. Food Chem Toxicol. 2020 Sep.
[34] Effect of omega-3 fatty acids and fish oil supplementation on multiple sclerosis: a systematic review. Welayah Ali AlAmmar et al. Nutr Neurosci. 2019 Aug.
[35] Chronic Inflammation in the Context of Everyday Life: Dietary Changes as Mitigating Factors. Margină D. et al. Int J Environ Res Public Health. 2020.
[36] World aging population, chronic diseases and impact of modifiable-metabolic risk factors. Dr. Dimitris Tsoukalas. International Congress of Rural Medicine, Tokyo, 2018.





