Why Your Thyroid Might Be Ruining Your Life (And You Don’t Know It)
Get Personalized Insights

Why Your Thyroid Might Be Ruining Your Life (And You Don’t Know It)
Thyroid dysfunction is the most common yet often underestimated condition that can significantly impact health and quality of life. Poor thyroid function encompasses a spectrum that includes: changes in thyroid structure on ultrasound, presence of nodules, hypothyroidism, hyperthyroidism, or the presence of antibodies against the thyroid (anti-TPO, anti-TG).
Individuals experiencing symptoms such as fatigue, low energy levels, reduced mental clarity, or difficulty regulating body weight are affected by poor thyroid function and may be at different points on this dysfunction spectrum. Some are diagnosed with hypo- or hyperthyroidism, others with Hashimoto’s thyroiditis, and some have elevated antibody levels. Often, individuals experience all the symptoms associated with poor thyroid function without these being reflected in standard tests.
It is common for someone to consult a doctor and have tests show normal thyroid function despite feeling unwell. Studies indicate that standard measurements (TSH, FT3, FT4) do not always correlate with symptoms. Thus, many people with thyroid dysfunction may have “normal” hormone levels.
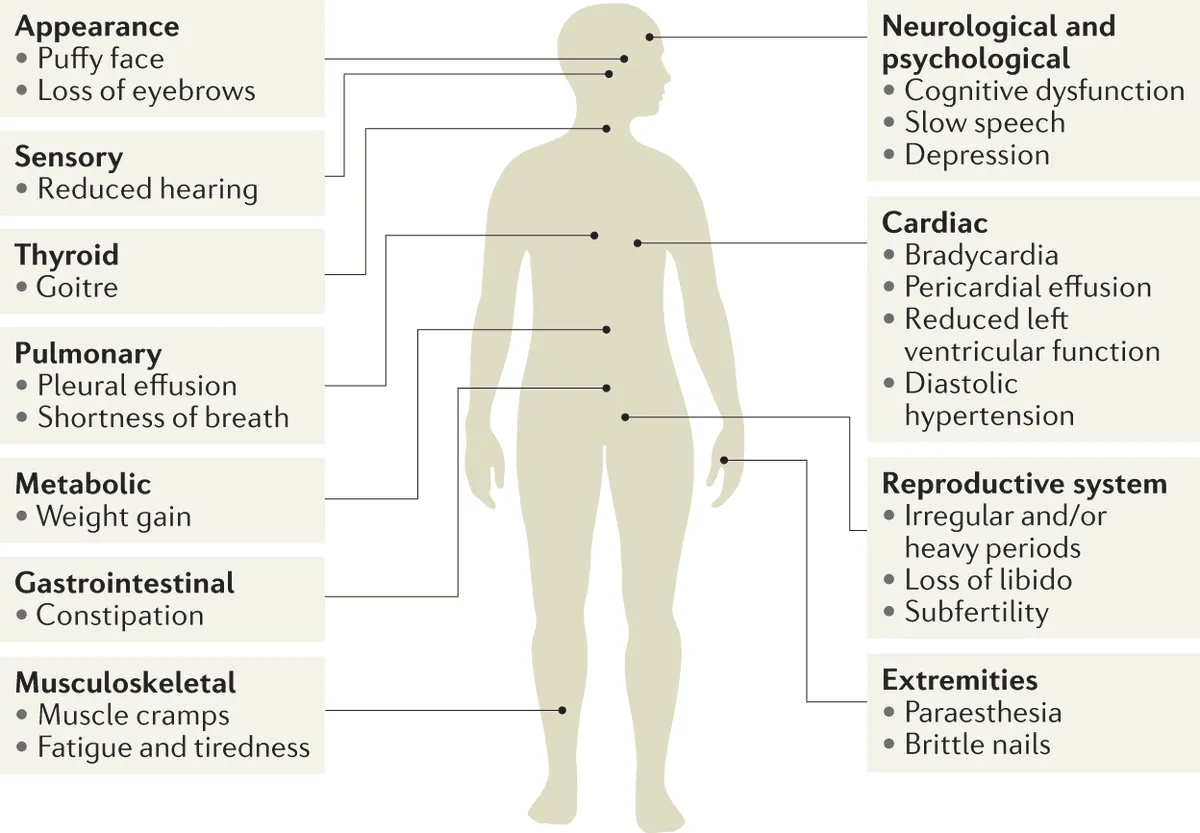
In all these cases, there is a common underlying factor that triggers and causes reduced or poor thyroid function, leading to symptoms such as:
- Fatigue and low energy levels
- Waking up tired despite adequate sleep
- Cold hands and feet
- Difficulty controlling weight
- Hair loss
- Reduced mental clarity
- Slow digestion, bloating, constipation
- Diffuse muscle pain
- Menstrual irregularities
- Infertility
All these symptoms share a common root: poor metabolic function.
Many may wonder how metabolism relates to poor thyroid function. In reality, metabolism is the primary culprit for the decline in thyroid function, as the thyroid regulates metabolism and vice versa.
Why the Body Fails to Produce Energy
Thyroid dysfunction stems from reduced energy production. When the body does not produce sufficient energy, it operates under constant strain. This reduced energy efficiency:
- Increases stress hormones
- Causes insulin resistance
- Strains the thyroid
- Negatively affects mood
- Impairs metabolic processes
- Contributes to weight gain
- Impacts cognitive functions
- Disrupts the hormonal system
- Is linked to infertility
- Causes hair loss and reduced bone density
- Accelerates aging
- Weakens immune system function
The factors causing reduced energy production are specific and can be addressed. These include:
- Deficiencies in vitamins and micronutrients
- Disruption of the gut microbiome and intestinal function
- Reduced ability to repair damage (chronic inflammation)
It is not widely known that nutrient deficiencies are the leading cause of disease worldwide.
When the body lacks essential components, it underperforms, the gut microbiome is disrupted, and the ability to combat oxidative stress (pollution, stress, alcohol, smoking, medications, or industrial chemicals) is diminished.
The human body requires 166 vitamins, minerals, amino acids, antioxidants, and other essential nutrients to carry out the metabolic processes that sustain life. When the body has all the necessary nutrients, it can produce energy, repair damage efficiently, and maintain a stable state of function (homeostasis).
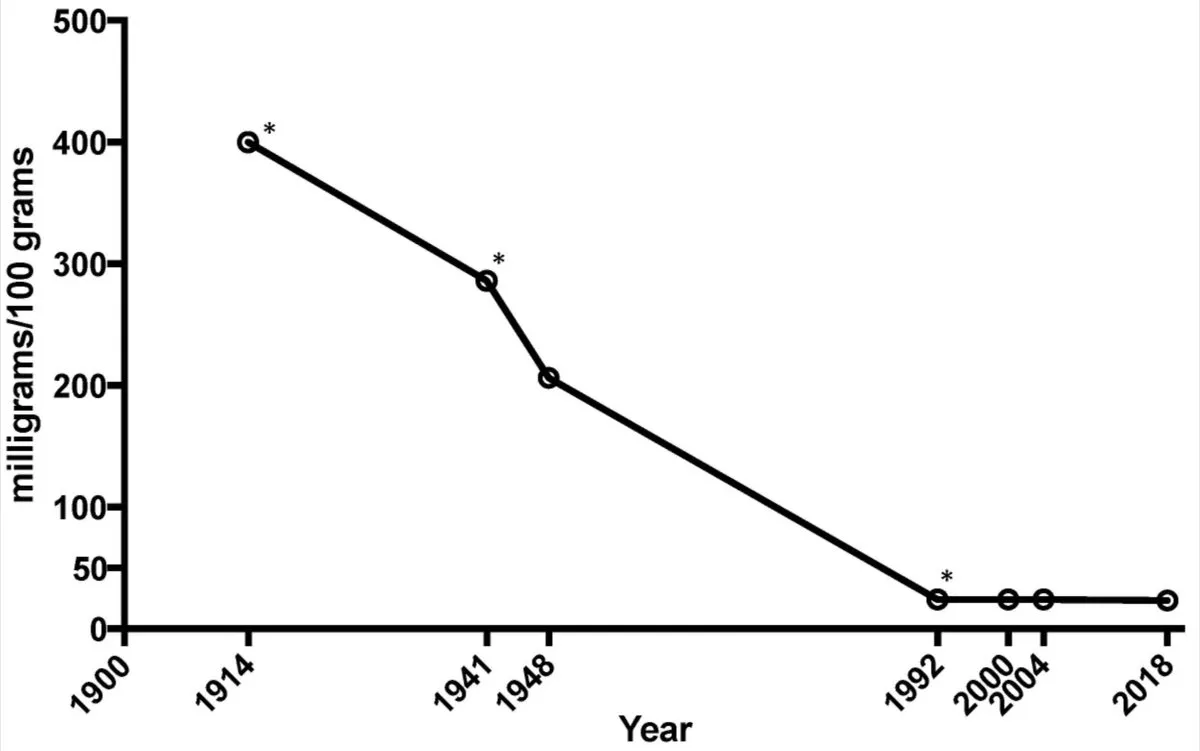
In developed countries, while we consume more calories, these often have low nutritional value. Even nutrient-rich foods (meat, eggs, dairy) contain 10-15 times fewer nutrients than they did 100 years ago. Over time, despite careful diet and lifestyle, the body accumulates deficiencies that disrupt its function.
Patients often assume these are merely signs of aging. In reality, they are not age-related and, if unaddressed, worsen over time.
While no abnormalities may be detected, the condition continues to deteriorate. To cope, the body increases stress hormones (cortisol, adrenaline) to produce energy through alternative mechanisms. However, stress hormones further impair thyroid function, cause insulin resistance, and intensify symptoms.
As the condition progresses, recommendations may include:
- Medications for cholesterol
- Medications for insulin resistance
- Antidepressants
- Weight-loss drugs
- Hormone replacement therapy (estrogens/progesterone for women, testosterone for men)
However, none address the root cause: thyroid dysfunction and low metabolism. If the factors leading to thyroid dysfunction are not addressed, the condition worsens, increasing the risk of:
- Autoimmune diseases
- Heart disease
- Bone mass loss
- Degenerative conditions (Parkinson’s, Alzheimer’s, osteoarthritis, atherosclerosis)
Many fail to understand what is happening in their bodies, attributing symptoms to age, genetics, or daily stress.
Identifying & Correcting Deficiencies
Deficiencies in vitamins, micronutrients, and metabolic disorders like insulin resistance are the primary drivers of disease, particularly regarding thyroid function.
The most reliable way to find them is comprehensive lab testing that maps whole-body biomarkers: metabolic status, thyroid function, inflammation, nutrient levels, cardiovascular risk, liver and kidney function, iron status, and more.
The advantage of in-depth lab testing is its ability to accurately identify deficiencies and metabolic disruptions, enabling targeted interventions to prevent or correct thyroid dysfunction. If deficiencies and metabolic disorders are not addressed, health continues to decline steadily.
A recent clinical study by our Chief Medical Advisor, Dr Dimitris Tsoukalas, published in BMJ Nutrition Prevention & Health, identified and corrected these factors in patients with thyroid dysfunction, autoimmune diseases, and chronic conditions, which improved quality of life in 95.7% of cases.
When deficiencies and metabolic disorders were identified and corrected in patients with Hashimoto’s thyroiditis, hypothyroidism, hyperthyroidism, diabetes, insulin resistance, cardiovascular diseases, arthritis, psoriasis, lupus, and other autoimmune conditions patients reported:
- 95.7% improved quality of life (energy, sleep, gut health)
- 89% sufficient energy (up from 31%)
- 87% improved gastrointestinal function (up from 27%)
- 80% absence of pain (up from 40%)
- 76% better stress management (up from 24%)
- 82% good stamina and physical condition (up from 27%)
We often forget that the body operates according to specific requirements. The further we deviate from these, the worse our health becomes, leading to conditions we then try to treat without addressing the root causes.
Conversely, the closer the body functions to these requirements, the better our health. Until recently, identifying deviations from normal function was challenging.
Comprehensive lab testing accurately detects these deviations and guide interventions to correct deficiencies, lifestyle, and diet, addressing the true root causes of disease.
Resolving metabolic disorders, correcting deficiencies in vitamins and other elements, enhancing thyroid function, boosting metabolism, and regulating weight to normal levels fundamentally improve health outcomes and quality of life.
References
- Sarandi, E., Tsoukalas, D. et al. Identifying the metabolic profile of Hashimoto’s thyroiditis from the METHAP clinical study. Sci Rep 15, 12410 (2025).
- Branca, F. et al. Transforming the food system to fight non-communicable diseases. BMJ, 28 January 2019.
- Workinger, J.L., Doyle, R.P., Bortz, J. Challenges in the Diagnosis of Magnesium Status. Nutrients, 2018.
- Magee, P.J., McCann, M.T. Micronutrient deficiencies: current issues. Proceedings of the Nutrition Society, 2019.
- Tsoukalas, D., Sarandi, E., Fragoulakis, V. et al. Metabolomics-based Treatment for Chronic Diseases: Results from a Multidisciplinary Clinical Study. BMJ Nutrition, Prevention & Health, 2025.





