Insulin Resistance: A Metabolic Disorder Leading to Extreme Fatigue & Chronic Inflammation in Patients with Autoimmune Disease
Get Personalized Insights

Insulin Resistance: A Metabolic Disorder Leading to Extreme Fatigue & Chronic Inflammation in Patients with Autoimmune Disease
Insulin resistance, a key metabolic disorder, is often an underlying factor in many issues experienced by patients with autoimmune diseases.
Many patients with autoimmune diseases are often unaware that symptoms such as low energy levels, muscle and joint pain, mood fluctuations, and gastrointestinal disorders are directly linked to insulin resistance.
This condition disrupts the immune system's functioning and is closely linked to increased inflammatory episodes and deteriorating health in autoimmune diseases.
Metabolic factors significantly influence autoimmune diseases. Issues like insulin resistance and micronutrient deficiencies, such as vitamins, minerals, amino acids, fatty acids, and others, further compromise the health of individuals with autoimmune conditions [1-4].
Insulin Resistance and Autoimmune Diseases: Three Common Problems Linked to This Metabolic Disorder
1. Energy Deficiency and Fatigue
One of the most common symptoms in patients with autoimmune diseases is fatigue and lack of energy.
While fatigue is a natural signal that our body needs rest to recover and repair daily wear and tear, it typically manifests towards the end of the day or after intense physical or mental activity. It usually resolves with adequate sleep and rest.
However, in autoimmune patients, fatigue often appears progressively earlier in the day. Initially, tiredness may begin in the afternoon, but as the condition advances, it can occur by midday.
Fatigue and low energy result from micronutrient deficiencies and metabolic dysfunctions that impair the body’s ability to produce energy.
Insulin resistance, along with micronutrient deficiencies, impedes the burning of fat and slows down metabolism. As a result, the body's efficiency decreases, leading the individual to experience extreme fatigue and reduced endurance for physical activities.
2. Chronic Pain
Chronic pain is a defining symptom of autoimmune diseases such as rheumatoid arthritis, Hashimoto’s thyroiditis, systemic lupus erythematosus, Sjögren’s syndrome, inflammatory bowel disease, ankylosing spondylitis, psoriasis, and scleroderma.
Patients often experience joint and muscle pain (myalgia), abdominal pain, discomfort in the fingers, and bladder pain. Even simple daily actions like climbing stairs, opening a bottle, eating, or urinating, can become painful.
Insulin promotes inflammation and exacerbates pain. It acts as a growth factor, encouraging body cells to proliferate and aggravating inflammation. Insulin resistance suppresses healing mechanisms, accelerates tissue damage, and leads to chronic inflammation.
3. Gastrointestinal Dysfunction
Most patients with autoimmune diseases experience gastrointestinal issues. Common symptoms include constipation, diarrhoea, bloody stools, difficulty swallowing, abdominal bloating, and pain.
These symptoms result from inflammation of the intestinal wall, disturbances in gut motility, and imbalances in the gut microbiome. Alterations in the intestinal flora are known to worsen insulin resistance and disrupt immune system regulation [5–7].
Insulin Resistance
Produced by the pancreas, insulin is primarily known for its role in lowering blood sugar levels.
Upon eating, the pancreas releases insulin. This hormone then attaches to cells, signalling them to absorb glucose from the bloodstream, thereby reducing circulating glucose levels.
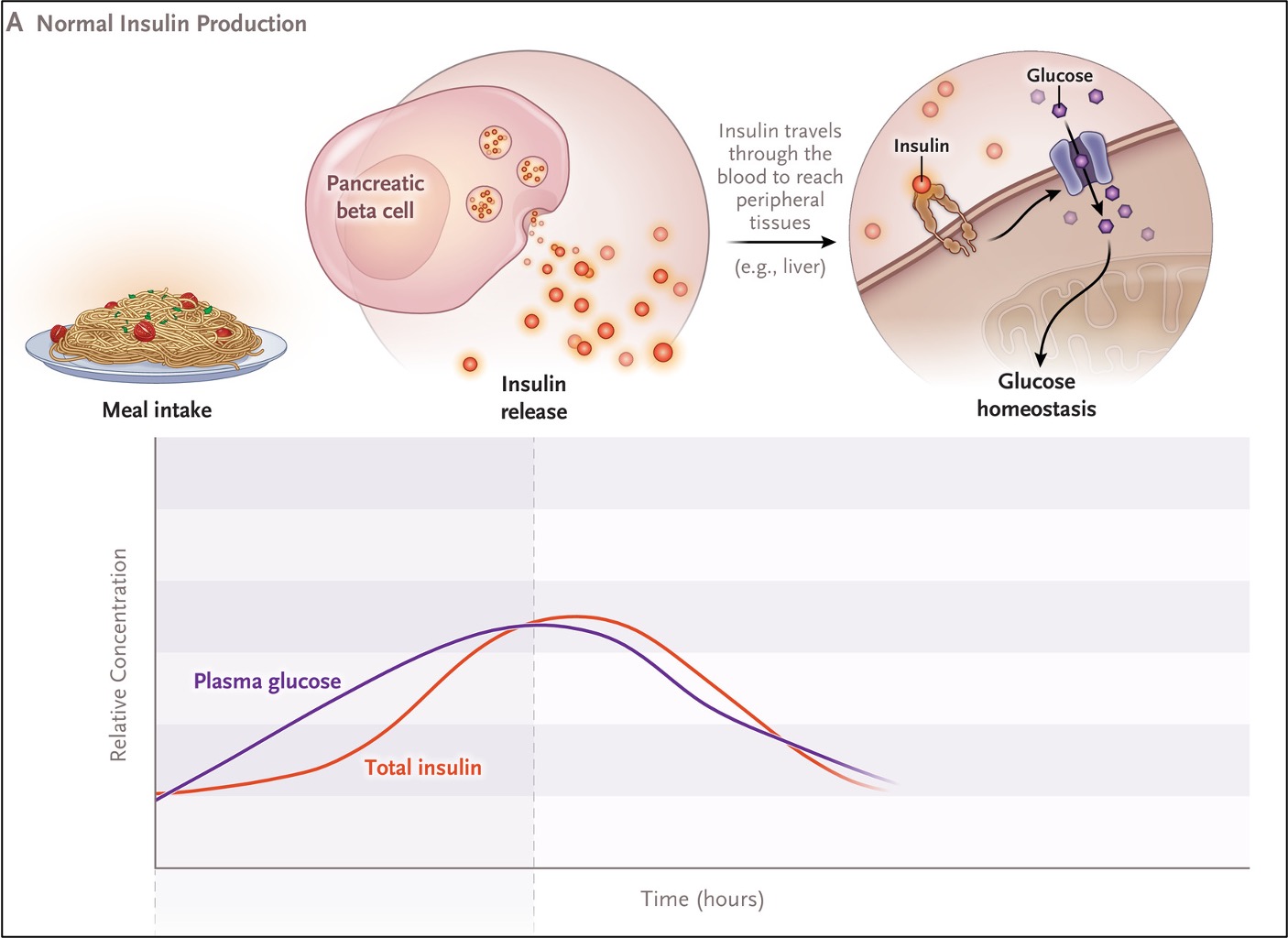
Insulin resistance occurs when cells in the liver, adipose tissue, and muscles try to protect themselves from excess glucose availability and become less responsive to insulin. The body must then produce progressively higher amounts of insulin to achieve the same biological effect.
Beyond maintaining blood sugar stability, insulin also regulates fat metabolism, energy production, and inflammatory processes that influence overall body function.
Elevated insulin levels intensify inflammation, exacerbate flare-ups in autoimmune diseases, contribute to the formation of atherosclerotic plaques in blood vessels, increase the risk of cancer development and the onset of diabetes.
Micronutrient Deficiencies & Insulin Resistance
Insulin resistance is a leading cause of disease today. When combined with marginal micronutrient deficiencies, it plays a central role in the development and progression of autoimmune disorders.
A sedentary lifestyle, combined with frequent consumption of processed foods that trigger increased insulin release, can lead to marginal deficiencies in vitamins and micronutrients.
These nutrients are essential for the proper functioning of insulin receptors. Over time, this progressively diminishes the cells' ability to respond effectively to insulin.
Micronutrients play a crucial role in the chemical reactions essential for sustaining life, collectively known as metabolism or metabolic processes.
Insulin resistance, a key metabolic disorder, significantly influences various bodily functions. It affects energy production, immune and hormonal balance, fertility, mood regulation, body weight management, and numerous other processes within the human body.
These marginal nutrient deficiencies often go unnoticed for years until the onset of a disease. They are challenging to detect with common lab tests and thus described as 'Hidden Hunger.'
For healthy metabolic functioning and resolution of insulin resistance, sufficient intake of vitamins, minerals, and micronutrients is essential [11–16]:
- For normal insulin secretion and function: magnesium, chromium, B-complex vitamins, vitamin K2, vitamin D3, and probiotics.
- For proper healing of skin and tissues: vitamin C, zinc, vitamin E, amino acids, antioxidants, vitamin D3.
- For controlling chronic inflammation: omega-3 fatty acids, vitamin C, vitamin D3.
- For healthy immune system function: vitamin D3, vitamin C, omega-3 fatty acids, probiotics, zinc.
Deficiencies in these specific micronutrients are directly linked to autoimmunity. Such deficiencies compromise health, promote insulin resistance, delay tissue repair, and promote chronic inflammation.
Specialised Tests for Individuals with Autoimmune Conditions
It is encouraging that lifestyle factors, micronutrient deficiencies, and diet—which can be identified and corrected—can improve the course of autoimmune diseases.
It is essential for patients with autoimmune diseases and metabolic disorders to identify the precise deficiencies affecting their health, as these are directly connected to insulin resistance.
Until a few years ago, precisely detecting deficiencies and the causing factors of metabolic disturbances like insulin resistance was challenging with ordinary tests. This led to reliance on general guidelines with limited efficacy.
Comprehensive lab testing that assess several functions of the body now provide a much more accurate picture of the deficiencies and metabolic disorders affecting an individual’s health.
These tests are not routinely performed during standard checkups. They are highly specialised and significantly more advanced, typically available only in select private clinics.
Kyma’s comprehensive lab panel measures the exact deficiencies, enabling a targeted health plan to address insulin resistance and improve overall health [3,4,17,18].
This panel includes more than 90 biomarkers directly related to an individual’s health status.
The tests identify deficiencies in vitamins and other elements associated with:
- Insulin resistance
- Carbohydrate metabolism
- Lipid metabolism
- Inflammation management
- Energy production
- Gut microbiome condition
- Immune system function
- Hormonal system function
The results are accompanied by a tailored health plan for each individual, while ongoing medical monitoring should be carried out by their primary care provider.
The protocols are based on the individual’s unique test findings and typically includes vitamins, micronutrients, dietary recommendations, and lifestyle modifications.
Because micronutrient deficiencies accumulate over time, their correction requires patience and consistent effort. Conducting these tests is the first step; the care team then formulates an individualised care plan based on the results.
The individual implements the personalised plan to address their condition and restore health. This process requires time, effort, and continuous followups by our health coaches. Although improvements can often be noticed early, significant changes usually occur within 6–8 months, with full stabilisation of metabolic function typically achieved after one year.
Correcting insulin resistance through interventions that address lifestyle, deficiencies, and nutrition transforms the health trajectory:
- Reduces fatigue and enhances energy levels
- Improves metabolism, reduces body weight and visceral fat
- Significantly improves daily life for individuals with chronic inflammatory diseases like Hashimoto's disease, psoriasis, rheumatoid arthritis, ulcerative colitis
- Reduces the risk of cardiovascular disease and diabetes
- Improves sugar and lipid metabolism
- Reduces inflammatory flare-ups
Our clinical experience has shown that correcting deficiencies in vitamins and other elements, restoring metabolism, and regulating weight to normal levels radically changes the health course in individuals with insulin resistance for the better, improving their quality of life from a state of constant deterioration to one of consistent improvement [3,4,17-19].
Timely intervention to restore these factors is essential to halt further deterioration and promote lasting recovery.
Bibliographic References
[1] Insulin Resistant Pathways are associated with Disease Activity in Rheumatoid Arthritis and are Subject to Disease Modification through Metabolic Reprogramming; A Potential Novel Therapeutic Approach," Lorna Gallagher Sian Cregan Monika Biniecka, et al. Arthritis and Rheumatolology. Dec. 16, 2019.[2] Chronic Inflammation in the Context of Everyday Life: Dietary Changes as Mitigating Factors. Margină, D.; Ungurianu, A.; Purdel, C.; Tsoukalas, D.; Sarandi, E.; Thanasoula, M.; Tekos, F.; Mesnage, R.; Kouretas, D.; Tsatsakis, A. Int. J. Environ. Res. Public Health 2020, 17, 4135.
[3] Targeted Metabolomic Analysis of Serum Fatty Acids for the Prediction of Autoimmune Diseases. Dimitris Tsoukalas, Vassileios Fragoulakis, Evangelia Sarandi et. al. Frontiers in Molecular Biosciences, Metabolomics, 2019.
[4] Prediction of Autoimmune Diseases by Targeted Metabolomic Assay of Urinary Organic Acids. Dimitris Tsoukalas et al. Metabolites. 2020 Dec 8.
[5] Gut Microbiota as a Trigger for Metabolic Inflammation in Obesity and Type 2 Diabeteσ. Torsten P. M. Scheithauer et al. Front. Immunol., 16 October 2020.
[6] Insulin resistance per se drives early and reversible dysbiosis-mediated gut barrier impairment and bactericidal dysfunction Author links open overlay panelDalaleGueddouri et al. Molecular Metabolism, March 2022
[7] Metabolic syndrome, autoimmunity and rheumatic diseases Gabriela Medina et al. Pharmacol Res . 2018
[8] Hidden Hunger in the Developed World. Biesalski HK. The Road to Good Nutrition. Basel, Karger, 2013, pp 39–50 https://doi.org/10.1159/000355992
[9] Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. Bruce N. Ames. PNAS 2006. https://www.pnas.org/content/pnas/103/47/17589.full.pdf
[10] Prolonging healthy aging: Longevity vitamins and proteins Bruce N. Ames PNAS October 23, 2018. https://www.pnas.org/content/115/43/10836
[11] Dietary micronutrients in the wake of COVID-19: an appraisal of evidence with a focus on high-risk groups and preventative healthcare. McAuliffe S, Ray S, Fallon E, et al. BMJ Nutr Prev Heal 2020:bmjnph-2020-000100.
[12] Insulin Resistance and Vitamin D Deficiency: A Link Beyond the Appearances. Valentina Trimarco et al. Front. Cardiovasc. Med., 17 March 2022
[13] Role of Minerals and Trace Elements in Diabetes and Insulin Resistance Pallavi Dubey et al. Nutrients. 2020
[14] Effects of Magnesium Deficiency on Mechanisms of Insulin Resistance in Type 2 Diabetes: Focusing on the Processes of Insulin Secretion and Signaling Krasimir Kostov Int J Mol Sci. 2019
[15] Effect of supplementation with vitamins D3 and K2 on undercarboxylated osteocalcin and insulin serum levels in patients with type 2 diabetes mellitus: a randomized, double-blind, clinical trial J. I. Aguayo-Ruiz et al. Diabetology & Metabolic Syndrome August 2020
[17] Non-communicable Diseases in the Era of Precision Medicine: An Overview of the Causing Factors and Prospects. Dimitris Tsoukalas et al. Bio#Futures. Springer, Cham. May 2021.
[18] Micronutrient deficiencies in patients with COVID-19: how metabolomics can contribute to their prevention and replenishment. Dimitris Tsoukalas1,2 and Evangelia Sarandi2,3 BMJ Nutri Prev Heal. Nov. 2020; bmjnph-2020-000169
[19] Dietary factors in rheumatic autoimmune diseases: a recipe for therapy? Shani Dahan, Yahel Segal1 and Yehuda Shoenfeld. NATURE REVIEWS | RHEUMATOLOGY. 13 Apr 2017.





